Critical Care Physicians Treating COVID-19 Report High Stress Levels
September 3, 2020 | Posted by ABIM | Uncategorized
Researchers at the American Board of Internal Medicine (ABIM), Harvard Medical School and the Harvard University T.H. Chan School of Public Health recently published results of a survey conducted earlier this year aimed at better understanding the experiences of critical care physicians caring for COVID-19 patients across the United States.
The survey, conducted 4/23/20 – 5/3/20, invited 14,141 currently or previously board certified physicians in Critical Care Medicine to participate and 2,882 responded (20% response rate). The complete results can be found here.
While many physicians have shared stories about what it’s been like caring for patients during the pandemic, this study is the first of its kind to produce quantifiable data in a number of areas that illuminate the lived experience of physicians on the front lines:
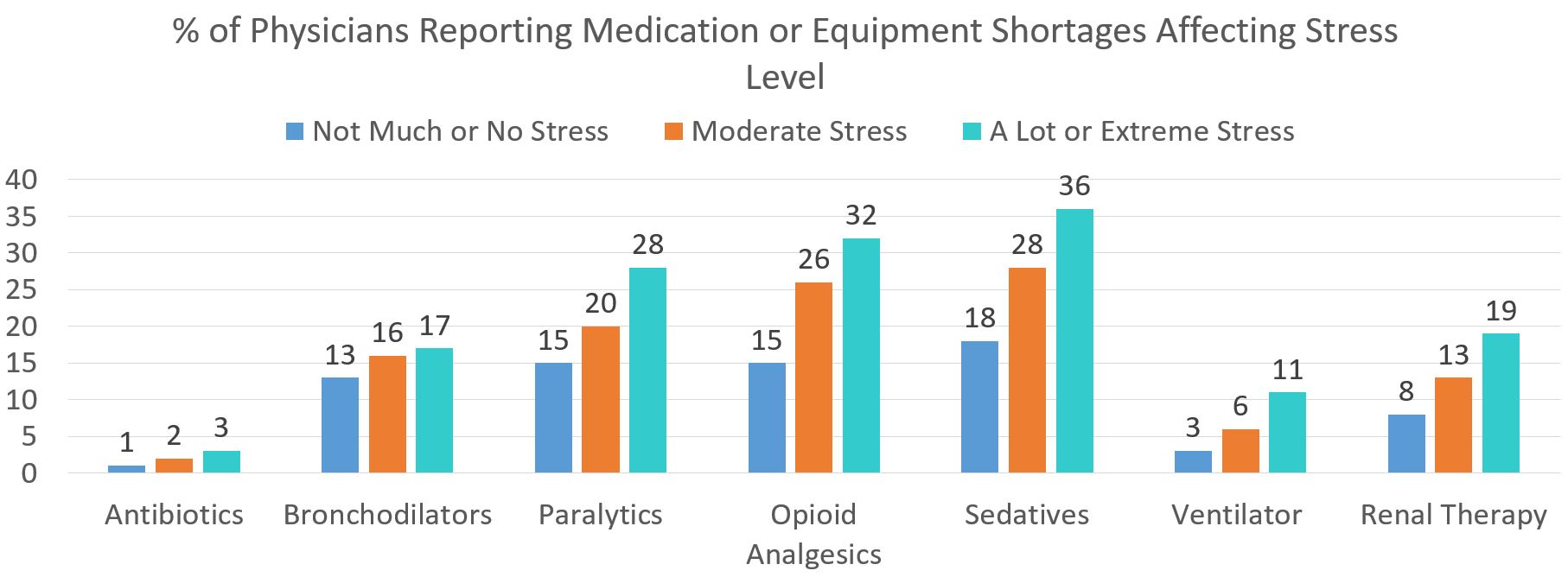
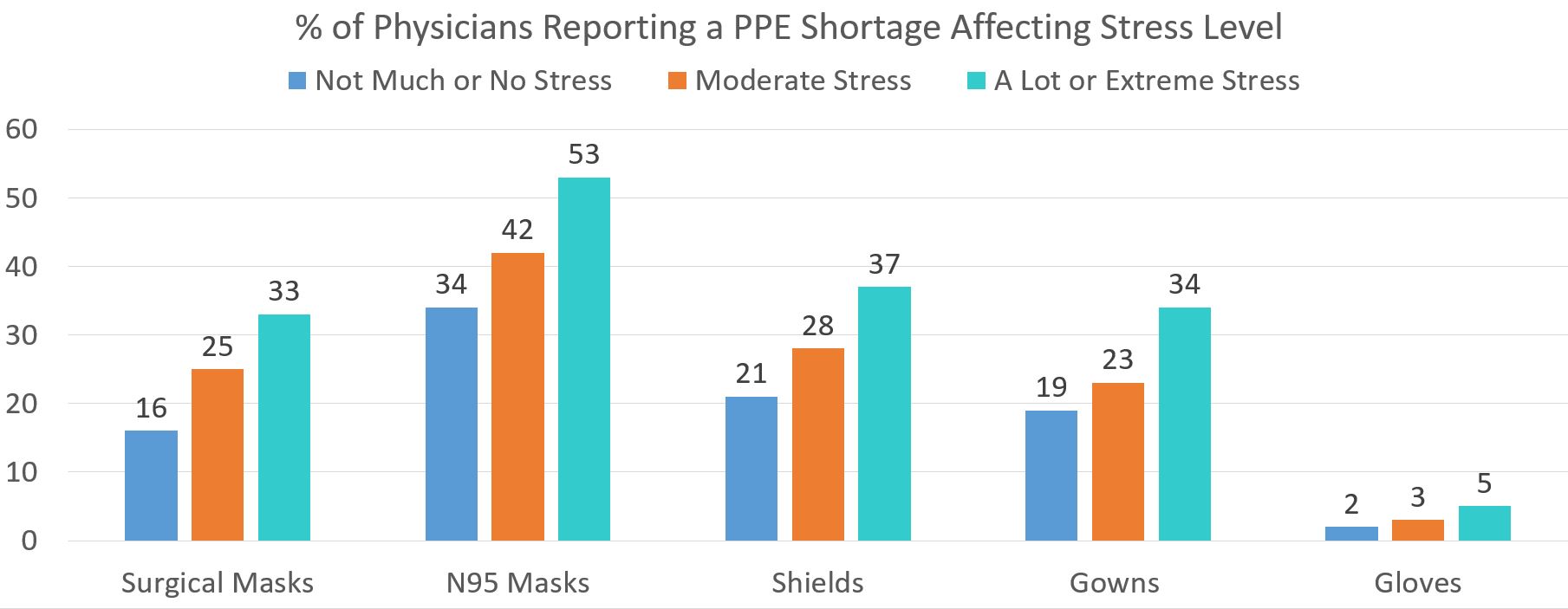
Shortages of medications, equipment, and PPE
Shortages that resulted in changes to clinical protocols for at least one class of medication typically used in the Intensive Care Unit (ICU) and Personal Protective Equipment (PPE) were reported by 43% and 52% of respondents respectively. Forty-five percent reported shortages in N95 masks, and 42% reported retaining their mask until soiled.
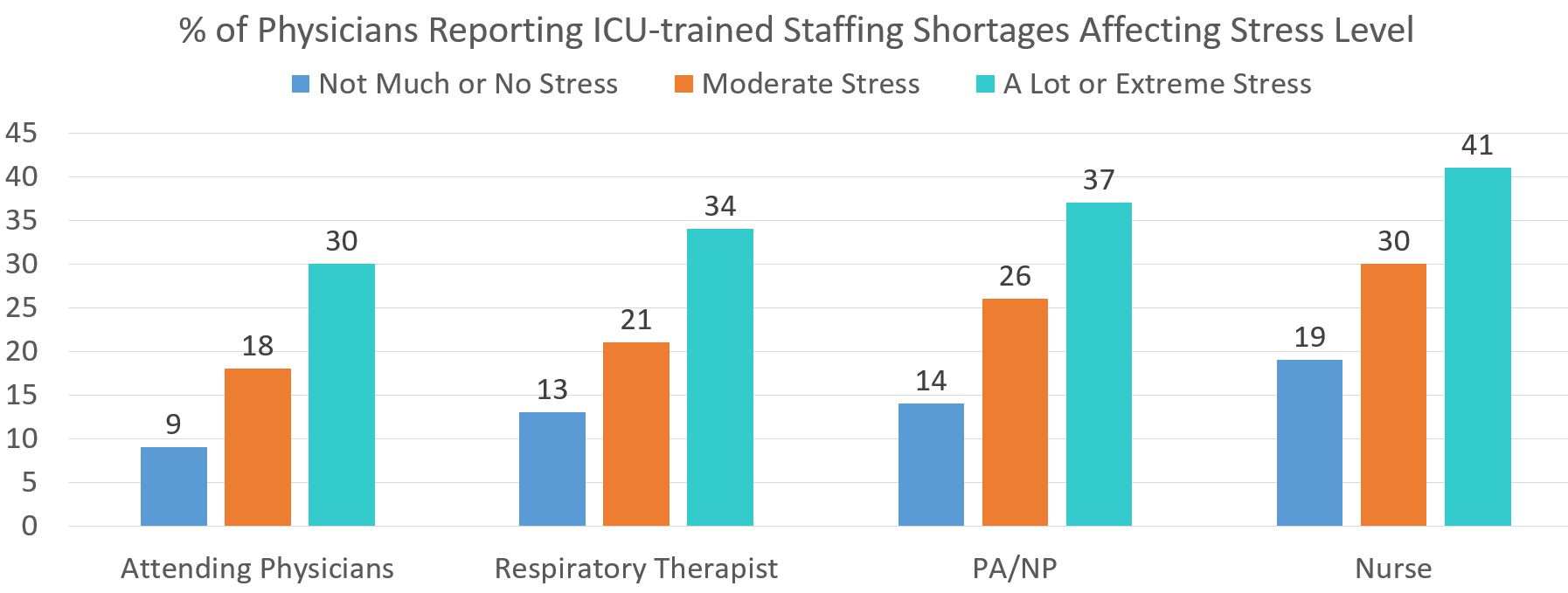
Inadequate staffing
Forty-eight percent of respondents reported at least one category of staffing in the ICU was inadequate or only adequate when including non-ICU trained staff.
High Levels of Physician stress
About 70% of physicians reported at least moderate levels of emotional distress or physical exhaustion from treating COVID-19 patients, including 26% who reported high levels of physical exhaustion and 29% who reported high levels of emotional distress.
Physician stress was significantly higher in COVID-19 hotspots and in areas experiencing shortages of medications, equipment, PPE and staff. Long wait times in receiving test results was also a contributing factor.
As the nation continues to grapple with the pandemic, the study authors call on policy makers to focus efforts on improving staffing levels, elevating shortages of medication and equipment and shortening testing times in order to reduce physician stress that might impact the availability and effectiveness of highly skilled critical care physicians. In addition, reducing the spread of the virus through contact tracing, social distancing and mask wearing would also reduce the stress faced by critical care physicians nationwide.
Considering the changing nature of the pandemic and continuing stress faced by critical care physicians, ABIM will conduct a follow up survey this fall.
How ABIM and the ABIM Foundation are Supporting Physicians During COVID-19
Recognizing the demands being placed upon physicians during the pandemic, ABIM has taken a number of steps in an attempt to reduce stress and provide more time and flexibility for physicians to maintain their certifications:
- No one will lose certification if they aren’t able to complete a Maintenance of Certification (MOC) requirement this year: Physicians that have an assessment, attestation or points due in 2020 will have until 12/31/21 to complete them.
- Physicians currently in their grace year will be afforded an additional grace year in 2021.
- Additional Knowledge Check-In dates will be provided for physicians in Critical Care Medicine and Hospital Medicine in 2021.
ABIM and the ABIM Foundation have also each contributed funds to #GetUsPPE to facilitate the delivery of more than 50,000 pieces of PPE to frontline physicians.
If you’re a physician experiencing a PPE shortage, you can be matched with a donor at getusppe.org.



